Hear my preacher, he has made understanding salvation easy....for the kids even. I want you to have eternal life, love Judy
Nothing wrong with believing in the invisible, supernatural world when we will spend the bulk of our existence there. Don't live for this messed up world, but the next. It's quite sensible to avoid eternal damnation and punishment. What have you got to lose?
Days of our Lives: Australian Version
Keeping my family updated about my life with a constellation of "insignificant" (not to me, to the medical system) symptoms called syndromes.
Paghttps://www.omf.ngo/wp-content/uploads/2020/07/Diagnosing-and-Treating-MECFS-Handout-V2.pdfes
Sunday, October 04, 2020
Wednesday, August 12, 2020
Friday, June 19, 2020
Sunday, June 14, 2020
Sunday, December 30, 2018
Wednesday, December 05, 2018
Tuesday, September 18, 2018
Kayak Man
 |
| He went fishing this way while he was here up Bell's Creek and saw a Sea Eagle |
We could have had a nice home-cooked meal together but Nick didn't want to bring him back. I even made a carrot cake to follow the schnitzels. It seems I enjoy being an old-fashioned Mum at times. Brett lives on frozen chicken rolls because they are cheap from the local IGA. She eats for nothing at her place of work and often brings Brett a meal. They don't do much together because of her night shift. And she works weekends. The last time Brett was here was when Nick got married Feb 2017 and Brett was best man. But now Nick and the mother of his new children are separated. It's all just drama and I don't have to be a part of it. Brett doesn't want to be either.
He says there is too much traffic here on the Coast for his liking. He likes it out there better but he does not like her job. He doesn't like his much either. It seems to involve macerators and pig shit. Welding with a putrid smell.
Thursday, September 13, 2018
Just stuff
Sunday, September 02, 2018
Local stuff
Volume problems: talk about the "Infiltration basin" and how rare it is to see a boat that big in our bit of the Pumicestone Passage.
Saturday, September 01, 2018
Heart Failure with preserved Ejection Fraction (HFpEF)
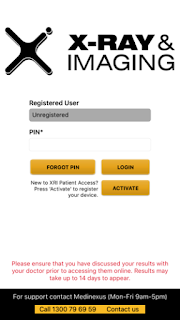
Having health records online may be a risk to privacy but the X-Ray and Imaging chain of imaging services offer an app when you go there for a procedure. I took the pamphlet and I signed up for the service so that I could get my results for my recent echocardiogram.
I saw Dr Jo before the results were available online anyway and I came away thinking that nothing much had changed except for the fact that that the pulmonary valve stenosis had reappeared in my life. The last I knew of it was that they had decided via a past echo that I didn't have one. It turns out that it has been on record again since 2011 when Dr Fleur must have ordered an echo. We spent time discussing this at my doctors appointment because Dr Jo was also unaware. Nevertheless it is only a minor stenosis. Everything came across as minor the way Dr Jo gave me the results..... the slight mitral valve weakness, the minor pulmonary valve narrowing and some diastolic abnormality that I barely took notice of because she said that the main thing was that I had a good ejection fraction of 65%. I did not realise the significance of that. It sounded all pretty "normal" or rather "benign" like my murmurs have been described in the past.
I have known for years that my diastolic blood pressure was too low and I have been surprised that no-one bothers to look at it even when I have provided charts of readings. It is always the top blood pressure reading they care about and it has been getting up rather high for me, over 140, lately but only at the doctors. At home it has been higher than normal though. I have also been carrying fluid around my lower legs and feet. That's why I had the echo, for pedal edema. I've been getting a lot of imprint marks from even loose socks and my boots on my legs and out-of-shape dispersions of fluid after I take them off. Dr Jo did see a similar raised area when I was there. It all got confused with my right foot being larger but later I remembered I had indeed dropped something heavy on my foot. The more general swelling seemed to come upon me when I went for slightly inclined walk up to the surf-life saving tower at Currimundi Lake. I could also feel fluid in my fingers that day. My knees have felt tight on bending and I have wondered if it was fluid in there too. Anyway I've noticed the puffiness in low places since that day. I was there with a couple of other ladies who have fibro and/or cfs.
The little conversation group we had formed on Facebook had been trying to get together face-to-face since the May 12 Awareness Day event. All but Anne (the one on the right) had to miss that due to not being well enough. It was the first time we had heard of something local to participate in. The May event was in support of #MEAction.
Two other ladies could not make it to our own little get together in July but they live beyond Caloundra in Buderim. Small distances matter when you have limited spoons. We have another lady in Ningi which is too far for us but her hubby gets her around sometimes. She came to meet me at a birthday gathering I had at the RSL one year.
Anyway getting back to the report, it states quite clearly that I have grade 2 diastolic dysfunction and Wikipedia defines that as:
There are four basic Echocardiographic patterns of diastolic heart failure, which are graded I to IV:
- The mildest form is called an "abnormal relaxation pattern", or grade I diastolic dysfunction. On the mitral inflow Doppler echocardiogram, there is reversal of the normal E/A ratio. This pattern may develop normally with age in some patients, and many grade I patients will not have any clinical signs or symptoms of heart failure.
- Grade II diastolic dysfunction is called "pseudonormal filling dynamics". This is considered moderate diastolic dysfunction and is associated with elevated left atrial filling pressures. These patients more commonly have symptoms of heart failure, and many have left atrial enlargement due to the elevated pressures in the left heart.
Grade III and IV diastolic dysfunction are called "restrictive filling dynamics". These are both severe forms of diastolic dysfunction, and patients tend to have advanced heart failure symptoms:
- Class III diastolic dysfunction patients will demonstrate reversal of their diastolic abnormalities on echocardiogram when they perform the Valsalva maneuver. This is referred to as "reversible restrictive diastolic dysfunction".
- Class IV diastolic dysfunction patients will not demonstrate reversibility of their echocardiogram abnormalities, and are therefore said to suffer from "fixed restrictive diastolic dysfunction".
I also have the left atrial enlargement.
I also have plenty of breathlessness. I was blaming the ME/CFS. However currently I am experiencing a high number of palpitations and it has been going on for weeks. Everything could be worse since going on the Olanzapine. I have had these heart symptoms in the past including pain in a very focussed area under my breast. I would call them pains, rather than one continuous pain. I have had it all before and it has all gone away after a season of it. I usually go on the Deralin but lately I noticed that I have been too dizzy on it and that I just don't feel like it is helping properly. Surely it slows down the heart palpitations, even can cure them but...lately my bottom blood pressure has been so low on it that all it is doing is widening my pulse pressure (the difference between the top and bottom) and when that happens I do not feel good. Helping in one way and making things worse in another. I have not actually told anyone about it. I have just tended to put up with the heart palpitations instead of taking the Deralin. I think I need a heart doctor. Why wouldn't Dr Jo suggest it that day? All I can think of is that it used to be thought that an ejection fraction above 50 or 60 meant that there was nothing wrong but now days they acknowledge a kind of heart failure that still preserves the ejection fraction, which means its systoles doing their pumping-out are fine. It is called diastolic dysfunction or diastolic heart failure but it is heart failure with preserved ejection fraction (HFpEF). Wikipedia goes on to say that there are few treatment plans for this kind of heart failure, except for diuretics to bring down the fluid levels in the legs or other places. It seems to be emerging as an ever increasing problem but insufficient research has been done. Where have I heard that before?
But there have been studies on older adults without systolic hypotension and with a wide pulse pressure, showing that isolated diastolic hypotension was associated with a significant increased risk of new-onset heart failure. Reference: Guichard et al available at https://www.ahajournals.org/doi/abs/10.1161/circ.122.suppl_21.A19925
The word "isolated" just means in the absence of.
Heart failure with preserved ejection fraction (HFpEF) is an emerging epidemic and there’s no pharmacotherapies yet proven to be useful for it,.......
Please add any relevant papers that you have come across in the comments section below.
Friday, August 24, 2018
"PAIN Making" written by Derek Morrison
‘THE ONGOING ADDITION OF DOCTORS’.
Today, here in Australia and around the world patients are being not only harmed but disabled due to the continued use of ‘off-label’ Injectable chemicals into the cerebrospinal fluid of the spine without Regulatory Approval. Epidural steroid injections for instance are a classic example of this today through such being used on ill-informed or non-informed unsuspecting patients and in some case directly ‘ordered by Insurance Companies’ to “hopefully” improve their moveability and able them to return to the workforce. Those that carry out these procedures have ‘also’ been ‘mixing’ two or more of these ‘off label’ toxic chemicals together, and injecting them Intrathecally into the patients without any awareness such was safe or had Regulatory Approval.
The question is ‘why’ have they been allowed to do so for decades without being challenged, “is such safe”??? The answer to this, is when such injections started way back in the early 1920’s in fact 1921 there were NO regulatory requirements Governments placed the trust and expertise in the hands of the Medical Profession without any checks and balances in place. In fact, the first injectable toxic chemical used as a dye in x-rays soon led to Chemically Induced Adhesive Arachnoiditis within the subarachnoid space, [spine] and due to such was stopped not by the Government but by the end-users themselves, the Doctors injecting such into the patients. This was due not so much for the welfare of the patients, but for ‘self protection’ legally.
The American FDA being the World Regulatory of new drugs had in place by the early 1900s a set regulatory requirements known as a New Drug Application [NDA] for Companies wishing to submit a new drug for Marketing. What was NOT in place was a set regulatory requirements for Companies wishing to submit an application for a General Marketing License for diagnostic radiographic x-ray toxic contrast mediums. [Dye] for until then end-users were using ‘Air’ in such procedures. [“Air is cheap”]
A specific regulatory requirement on x-ray contrast mediums [dyes] never arrived until 1969 almost half a century later, due to the thalidomide issue, by this time the medical profession had injected this “dye” injuring close to 60 million patients throughout the world 20 million of these in the US and tens of thousands here in Australia without any knowledge of doing so. Why was this? Well those carrying out these injections were not ‘linked’ to the patent’s GP, Specialists and such like, furthermore, the development of chemically induced adhesive arachnoiditis is insidious. The slow damage to peripheral nerve roots and the related man-made disability for many [but not all] develops over time and a relationship to the cause, a past injection of what was deemed to be safe, was never considered.
Today, here in Australia and around the world the practice of ‘off-label’ use continues without any Governmental oversight or Regulatory approval of such practice in place. I believe not only these end-users need to be held accountable BUT also the Government Regulators, of each of the 107 Counties where it was used, sadly many of those once employed by these Government Regulators throughout the world are NOW working for the the Manufacturer’s or subsidiaries.
My Blog explains how many Australians today have been harmed by this unregulated x-ray dye and ‘other’ such injectable substances into the CSF of the spine [and elsewhere].
The first contrast medium causing horrendous pain and disability was lipiodol an x-ray oil based dye (1921-1946) then came Iophendylate Pantopaque or Myodil another oil base x-ray dye [1936 – 1996] causing chemically induced adhesive arachnoiditis.
Also, my research and that of others show that even the newer water base x-ray dyes cause chemically induced adhesive arachnoiditis and the related horrendous pain and disability.
It's clear today, what has happened and its cause, it's now up to you the reader to understand how this was allowed to happen.
PLEASE FORWARD TO OTHERS ESPECIALLY THE MEDIA.
Wednesday, August 22, 2018
Tuesday, August 21, 2018
Tuesday, August 14, 2018
Alan Watts ~ Go WIth It
I have to!
Labels:
#fibromyalgia,
#lyme,
#mecfs,
Alan Watts,
pain,
philosopher,
suffering
Subscribe to:
Comments (Atom)