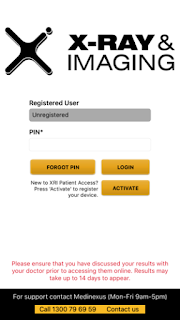
Having health records online may be a risk to privacy but the X-Ray and Imaging chain of imaging services offer an app when you go there for a procedure. I took the pamphlet and I signed up for the service so that I could get my results for my recent echocardiogram.
I saw Dr Jo before the results were available online anyway and I came away thinking that nothing much had changed except for the fact that that the pulmonary valve stenosis had reappeared in my life. The last I knew of it was that they had decided via a past echo that I didn't have one. It turns out that it has been on record again since 2011 when Dr Fleur must have ordered an echo. We spent time discussing this at my doctors appointment because Dr Jo was also unaware. Nevertheless it is only a minor stenosis. Everything came across as minor the way Dr Jo gave me the results..... the slight mitral valve weakness, the minor pulmonary valve narrowing and some diastolic abnormality that I barely took notice of because she said that the main thing was that I had a good ejection fraction of 65%. I did not realise the significance of that. It sounded all pretty "normal" or rather "benign" like my murmurs have been described in the past.
I have known for years that my diastolic blood pressure was too low and I have been surprised that no-one bothers to look at it even when I have provided charts of readings. It is always the top blood pressure reading they care about and it has been getting up rather high for me, over 140, lately but only at the doctors. At home it has been higher than normal though. I have also been carrying fluid around my lower legs and feet. That's why I had the echo, for pedal edema. I've been getting a lot of imprint marks from even loose socks and my boots on my legs and out-of-shape dispersions of fluid after I take them off. Dr Jo did see a similar raised area when I was there. It all got confused with my right foot being larger but later I remembered I had indeed dropped something heavy on my foot. The more general swelling seemed to come upon me when I went for slightly inclined walk up to the surf-life saving tower at Currimundi Lake. I could also feel fluid in my fingers that day. My knees have felt tight on bending and I have wondered if it was fluid in there too. Anyway I've noticed the puffiness in low places since that day. I was there with a couple of other ladies who have fibro and/or cfs.
The little conversation group we had formed on Facebook had been trying to get together face-to-face since the May 12 Awareness Day event. All but Anne (the one on the right) had to miss that due to not being well enough. It was the first time we had heard of something local to participate in. The May event was in support of #MEAction.
Two other ladies could not make it to our own little get together in July but they live beyond Caloundra in Buderim. Small distances matter when you have limited spoons. We have another lady in Ningi which is too far for us but her hubby gets her around sometimes. She came to meet me at a birthday gathering I had at the RSL one year.
Anyway getting back to the report, it states quite clearly that I have grade 2 diastolic dysfunction and Wikipedia defines that as:
There are four basic Echocardiographic patterns of diastolic heart failure, which are graded I to IV:
- The mildest form is called an "abnormal relaxation pattern", or grade I diastolic dysfunction. On the mitral inflow Doppler echocardiogram, there is reversal of the normal E/A ratio. This pattern may develop normally with age in some patients, and many grade I patients will not have any clinical signs or symptoms of heart failure.
- Grade II diastolic dysfunction is called "pseudonormal filling dynamics". This is considered moderate diastolic dysfunction and is associated with elevated left atrial filling pressures. These patients more commonly have symptoms of heart failure, and many have left atrial enlargement due to the elevated pressures in the left heart.
Grade III and IV diastolic dysfunction are called "restrictive filling dynamics". These are both severe forms of diastolic dysfunction, and patients tend to have advanced heart failure symptoms:
- Class III diastolic dysfunction patients will demonstrate reversal of their diastolic abnormalities on echocardiogram when they perform the Valsalva maneuver. This is referred to as "reversible restrictive diastolic dysfunction".
- Class IV diastolic dysfunction patients will not demonstrate reversibility of their echocardiogram abnormalities, and are therefore said to suffer from "fixed restrictive diastolic dysfunction".
I also have the left atrial enlargement.
I also have plenty of breathlessness. I was blaming the ME/CFS. However currently I am experiencing a high number of palpitations and it has been going on for weeks. Everything could be worse since going on the Olanzapine. I have had these heart symptoms in the past including pain in a very focussed area under my breast. I would call them pains, rather than one continuous pain. I have had it all before and it has all gone away after a season of it. I usually go on the Deralin but lately I noticed that I have been too dizzy on it and that I just don't feel like it is helping properly. Surely it slows down the heart palpitations, even can cure them but...lately my bottom blood pressure has been so low on it that all it is doing is widening my pulse pressure (the difference between the top and bottom) and when that happens I do not feel good. Helping in one way and making things worse in another. I have not actually told anyone about it. I have just tended to put up with the heart palpitations instead of taking the Deralin. I think I need a heart doctor. Why wouldn't Dr Jo suggest it that day? All I can think of is that it used to be thought that an ejection fraction above 50 or 60 meant that there was nothing wrong but now days they acknowledge a kind of heart failure that still preserves the ejection fraction, which means its systoles doing their pumping-out are fine. It is called diastolic dysfunction or diastolic heart failure but it is heart failure with preserved ejection fraction (HFpEF). Wikipedia goes on to say that there are few treatment plans for this kind of heart failure, except for diuretics to bring down the fluid levels in the legs or other places. It seems to be emerging as an ever increasing problem but insufficient research has been done. Where have I heard that before?
But there have been studies on older adults without systolic hypotension and with a wide pulse pressure, showing that isolated diastolic hypotension was associated with a significant increased risk of new-onset heart failure. Reference: Guichard et al available at https://www.ahajournals.org/doi/abs/10.1161/circ.122.suppl_21.A19925
The word "isolated" just means in the absence of.
Please add any relevant papers that you have come across in the comments section below.


No comments:
Post a Comment